I am born and trained in Germany. I started as staff physician at nuclear medicine at Haukeland University Hospital in Bergen/Norway in October 2005. Half a year later I was appointed adjunct associate professor at the Section of Radiology at the University of Bergen (UiB).
The section chief, the late professor Jarle Rørvik, had made a major investment in new teaching tools, including hand-coded multimedia lectures on the Internet in Flash® format and an interactive teaching website (Rabilda), and the Section for Radiology had just received the faculty’s study quality award. The expectations for my teaching were high, and I tried to do my very best: I created a large set of multimedia lectures on nuclear medicine using a new authoring tool (Articulate), and when I taught showing live cases on a dedicated nuclear medicine workstation in interactive format, not just still images in PowerPoint. In the beginning, I even carried my large and heavy diagnostic workstation into the lecture theatre and and set it up there. Still I faced constant complaints by my medical students that nuclear medicine was not relevant to them since they were to practice medicine as residents and general physicians, but not nuclear medicine specialists.
I started introducing humour as a key ingredient into my teaching sessions. My intention was as follows: (i) When I got my students to laugh they would miss for a short moment their dislike of my subject and I could slip across an important teaching point under their radar. (ii) Even if my students were to forget everything that I tried to teach them on nuclear medicine they should at least remember me as a colourful exponent of my rare discipline. – At the time I was quite convinced that my teaching was top-of-the-line until one of my best friends in Norway, a nuclear physician trained in Germany just like myself, attended one of my teaching sessions. I expected praise for my modern teaching, but she remarked that she could see that I was getting frustrated. This was to become the turning point in my teaching career; however I was still caught in the old curriculum.
The new curriculum in Bergen “Medicine 2017” and new learning management system (LMS) Canvas LMS launched by the University of Bergen at about the same time both turned out to be game changers. The new course module “Nuclear Medicine in Endocrinology” was the first in which in which I was given the chance to pull all the stops and introduce e-learning in a big way. I began recording a whole new set of new e-lectures. I had observed my children perusing YouTube. My new e-lectures adhered to the same standard by being shorter than ten minutes each. I combined my new e-lectures with an online readiness assessment test in the form of a short multiple-choice examination in Canvas LMS: Students had to pass the test before meeting me the next day. For the first time in ten years, my students attained the necessary foundational knowledge before attending my teaching. This relieved me of lecturing and freed time for discussion and reflection. “Nuclear Medicine 1.0” was rewarded with the Medical Faculty’s study quality price 2017. The immediate benefit of the price was that it I was allowed to teach “Nuclear medicine in Oncology” in the 10th term, a module that had been missing in the original curriculum.
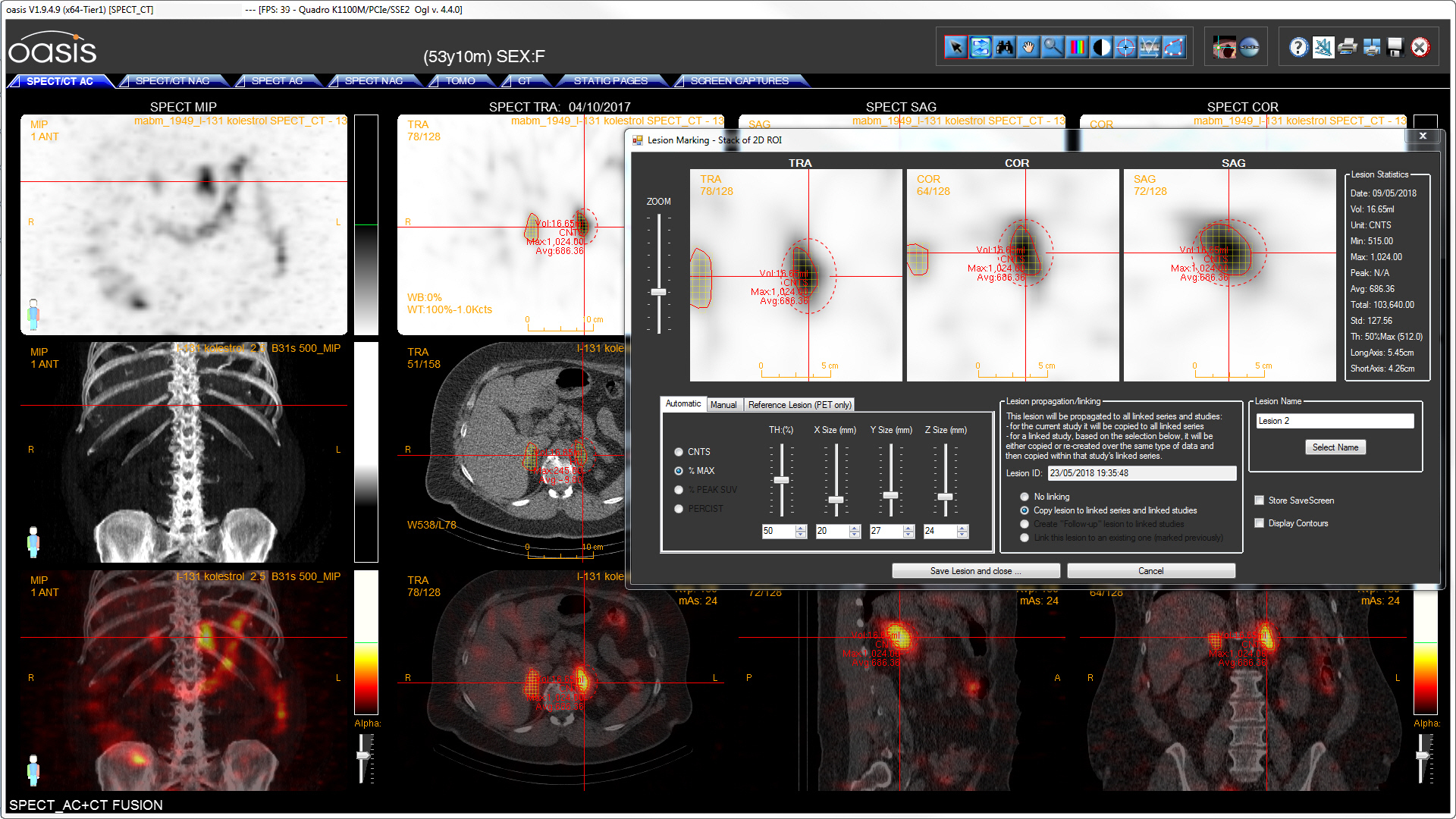
Most people would been happy with the price and the gained extra teaching time and moved on, I was happy and went into overdrive. “Nuclear medicine 1.5” was the introduction of a nuclear medicine station into the Objective Structured Clinical Examination (OSCE) at the end of the sixth term at the University of Bergen. Students were to show the examiner a PET/CT examination of a patient with lung cancer in native nuclear medicine software and diagnose the correct tumour stage and prescribe the appropriate treatment. To prepare students for the OSCE station, I created sets of multiple-choice questions in UiB’s Canvas LMS paired to five anonymized cases in our institutional teaching database. Under the OSCE examination, 96% of students passed in respect to the predefined standard [1].
Inspired by my mentor Robert Gray at the Department of Education UiB and Dee Fink and Elizabeth Barclay, whom both gave seminars in Bergen following Robert’s initiative, I was getting increasingly interested in the students’ perspective [2]. Traditional higher education is largely based on lecturing to transfer knowledge. Emphasis is laid on what the teacher does. However, the most important determinant for student success is what goes on in the students. While the amount of knowledge grows exponentially and old knowledge is steadily phased out, knowledge has become more accessible through the Internet and mobile devices. Therefore, it has become even more important than in the past to teach understanding of the underlying principles rather than cover all details, many of which will soon be superseded.
In the field of medical imaging, I claim that it also has become more important to teach skills rather than just knowledge. To succeed in a practical task such as navigating the human body in a PET/CT study creates student engagement. At the same time, it becomes easier for the student to absorb the essential underlying facts (Dee Fink: “foundational knowledge”). Students gain deeper understanding, which promotes more lasting teaching outcomes [1].
To get more insight of what goes on in the students while I am teaching, I introduced a classroom response system into my face-to-face teaching session [2]. This I called “Nuclear Medicine 2.0”. I supplemented this by establishing more frequent direct contact with individual students. – Recently I launched a new IT platform allowing students to browse PET/CT examinations in native format on their own personal computers while they were locked out from the hospital under the COVID pandemic [3]. To find out weaknesses in the implementation of the software and my teaching materials, I asked the first five students to share their computer screens with me. While I was talking to the students, I used the opportunity to ask the students how they felt when they were isolated from their fellow students and the patients in the hospital.
Teaching medicine at a University hospital is not only about medical students. Training junior physicians and other medical professions and guiding aspiring academic colleagues are just as important. Teaching always entails the risk that the student may become more proficient than oneself. This is how human culture works, and we should be proud if our own disciples surpass the limits of what we originally taught them.
All in all, I have become a nicer and more reflective teacher [4] than I was when I moved to Norway. I was surprised when the student graduates at UiB awarded me their price for the best lecturer in autumn 2019, especially since I had not taught them in their last year. I have to admit that my skills as a pedagogue at home are constantly criticised. Sutton and Huggy speculate that executives with teenage children are less prone to arrogance and delusions of grandeur. No matter how much respect their subordinates and adherents bestow on them, their teenage children will remain unimpressed and keep up their candour [5].
References
- Gulati A, Schwarzlmüller T, du Plessis E, Søfteland E, Gray R, Biermann M. Evaluation of a new e-learning framework for teaching nuclear medicine and radiology to undergraduate medical students. Acta Radiol Open. 2019;8:2058460119860231.
- Biermann M. Building an inclusive classroom – a blended course in Nuclear Medicine. UPED-Skrift. 2018;2018:1–8.
- Biermann M, Kanoun S, Davidsen T, Gray RJr. Teaching PET/CT to medical students under the COVID-19 lockout: Implementing a new freeware client server PET/CT viewer in the university network (Abstract; submitted). Eur J Nucl Med Mol Imaging. 2020;
- Brookfield S. Becoming a critically reflective teacher. Second edition. San Francisco, CA: Jossey-Bass; 2017.
- Sutton RI. The Asshole Survival Guide. New York, NY, US: Houghton Mifflin Harcourt; 2017.