Abstract
Nuclear medicine (NM) has been taught in the medical program at the University of Bergen (UiB) since 2006. Despite many incremental improvements in content delivery including a full set of online lectures since 2006, my teaching failed to captivate my target audience, leading to disappointing student responses over many years.
The new curriculum “Medisin 2015” introduced e-learning/blended learning based on UiB’s new learning management system (LMS) https://mitt.uib.no, while at the same reducing the volume of face-to-face (F2F) teaching. This forced me to redesign my teaching in NM from the ground up. Inspired by team-based learning, I introduced each course module by new succinct online-lectures, followed by an online readiness assessment test (RAT) in the LMS. To engage the entire audience during the F2F sessions, I not only taught with live case in interactive format as under the old curriculum but introduced a classroom response system. Finally, I shifted the focus from transferring knowledge to teaching PET/CT reading competency both in the third and the fifth year.
In the following I describe my development as a university teacher and outline my teaching philosophy.
Keywords:
Teaching; Nuclear medicine; Significant learning; Blended learning; Community of inquiry
This text is published in UPED-Skrift 10/2020 (Open Access).
1. Introduction
Nuclear medicine is the “medical specialty involving the application of radioactive substances in the diagnosis and treatment of disease.” (Rootwelt 2005). While factually correct, this definition of nuclear medicine is rather dry and uninspiring. Nuclear medicine has also been dubbed “unclear medicine” (Wictionary 2020). No wonder that teaching nuclear medicine to medical students is a major challenge!
I began teaching nuclear medicine shortly before becoming staff physician at the Department of Nuclear Medicine at Münster University Hospital in Münster/Germany in 2003. In 2005 I relocated to Bergen/Norway, joining the then minuscule nuclear medicine unit at Haukeland University Hospital.
Teaching nuclear medicine as new adjunct associate professor at the University of Bergen (UiB) turned out to be more difficult than I had envisaged. In retrospect, I began to realize that teaching and pedagogy had not had high status in the German academic system, which was all geared towards research and publications. It had been easy for me to outperform other teachers as expectations from German medical students had been low. Things were markedly different at the University of Bergen. Under the leadership of Professor Jarle Rørvik, the Section for Radiology had just received the faculty’s teaching quality award 2006 (Studiekvalitetsprisen). They had launched a series of nine multimedia online lectures (https://www.uib.no/radionett), and supplemented them by a newly developed interactive e-learning tool called RABILDA (Haagensen and Olsen 2003).
I tried hard to deliver nuclear medicine teaching at the same level of technical excellence. I launched a full set of multimedia lectures on nuclear medicine based on a new authoring tool (Articulate; https://articulate.com) already in summer 2006. In my seminars, I demonstrated original cases interactively in native diagnostic format. I even carried my diagnostic workstation into the lecture theater. I polished my Microsoft PowerPoint slides again and again. Still, I did not hit the nerve in my target audience. For years, I was haunted with poor student evaluations to the extent that I stopped reading them.
I began to see light when I took the course in University Pedagogy (https://www.uib.no/en/uped) in 2017. At the same time, a new medical curriculum (“Medicine 2015”) was phased in. Both transformed my teaching. In 2017, Nuclear medicine received the Medical Faculty’s teaching quality prize. In December 2019, I was honored with the “Best Lecturer” award by the student graduates.
What had changed? I claim: I myself as a teacher, but also my teaching environment.
Teaching does not happen in a vacuum, but is embedded in an institutional context (Biggs and Tang 2011). To outline my development as an academic teacher, I therefore start by describing the teaching setting followed my teaching initiatives. In the second part, I present some of the theory that has guided me, and I will conclude with my plans for further development.
2. Teaching under the old curriculum “Medicine 2005”
Under the “old” medical curriculum at UiB called “Medicine 2005”, radiology and nuclear medicine were taught in two blocks in the 3rd and 6th years. Teaching in the 3rd year commenced with twelve 45-minute plenary lectures including two on nuclear medicine. This was supplemented by a series of 90-minute seminars including two on nuclear medicine. Teaching in the 6th year followed the same pattern, but minus lectures and in groups of 20 students rather than 40. At the end of the 6th year, every student had to pass a 30-minute oral examination. Students had to read and interpret real radiology cases using live images in the departmental Picture Archival and Communication System (PACS), which I witnessed them to do with aplomb. In 2009, the examination was modified to include 5 multiple choice questions (MCQ) on nuclear medicine that the students solved on paper under the oral examination. At about that time, cases were no longer viewed live in the PACS but in the form of PowerPoint slides due to increasingly strict data protection rules.
Under the old curriculum, I spent a lot of time and effort on optimizing content delivery: I polished my PowerPoint presentations with ever more lucid diagrams and succinct bullet lists. I demonstrated cases live using diagnostic nuclear medicine software. To increase student engagement under my seminars, I developed an elaborate technique of Socratic questioning: I passed a second laser pointer to the audience, and asked a carefully planned sequence of questions to the student who was in possession of the pointer (Biermann 2018).
Despite all my efforts, my teaching went flat. Student evaluations (when I cared to read them) were poor – particularly when I related them to the amount of work that I spent on preparing my teaching. Most students complained that nuclear medicine was not relevant for general physicians and that I demanded too much (Biermann 2018).
3. The new curriculum
The new curriculum “Medicine 2015” brought a whiff of fresh air. It included a number of welcome changes: (i) Teaching embedded in a clinical context (such as endocrinology and oncology), (ii) New focus on e-learning with the launch of the Canvas Learning Management System (LMS) (https://mitt.uib.no), (iii) Objective structure clinical examinations (OSCE) at the end of the 3rd and 6th years, and (iv) Elective courses.
Ad (i): Under new curriculum “Medicine 2015” medicine is no longer taught according to medical specialty but in thematic blocks such as “circulation”, “central nervous system”, “endocrine system”, or “cancer”. Radiology and nuclear medicine are introduced in a series of lectures in the 5th term just as under the old curriculum. However, starting with the 6th term, both subjects are taught in forms of modules attached to the larger thematic blocks. While nuclear medicine kept one introductory 90-minute seminar in the 5th term, two new 90-min modules were introduced in the higher years: “Nuclear medicine in endocrinology” in the 8th term and “Nuclear medicine in oncology” in the 10th term.
Ad (ii): UiB launched a new e-learning system, the Canvas Learning Management System (LMS) (https://mitt.uib.no).
Ad (iii): OSCE is a practical examination which consists of a set number of “stations” in which a student has to solve a predefined medical problem within a set time period (e.g. 8 min) against a predefined “objective” standard according to a standardized checklist with explicit criteria (Gulati et al. 2019).
Ad (iv): Students can choose elective courses of either two or four weeks’ duration after completing their third year.
Before I explain how I innovated my teaching under the new curriculum, let us reflect on learning outcomes.
4. Learning outcomes
Under the new medical curriculum “Medicine 2015” at the University of Bergen, learning objectives for radiology and nuclear medicine include both foundational knowledge (such as the principles underlying image generation and knowing typical image findings) and practical skills such as being able to perform an ultrasound examination and read and interpret typical radiological examinations.
The inclusion of practical skills in medical imaging may be controversial, and indeed, in some of our surveys, students have questioned the value of practical exercises in nuclear medicine (Biermann et al. 2020a). We however consider practical skills a vital part of nuclear medicine education for the following reasons (Biermann et al. 2020a submitted, minor revision):
- On a pedagogical level we adhere to Fink’s concept of aiming for “rich” learning outcomes to promote significant learning (Fink 2013). This entails “learning by doing”. Doing is on a higher cognitive level than mere reproduction of foundational knowledge.
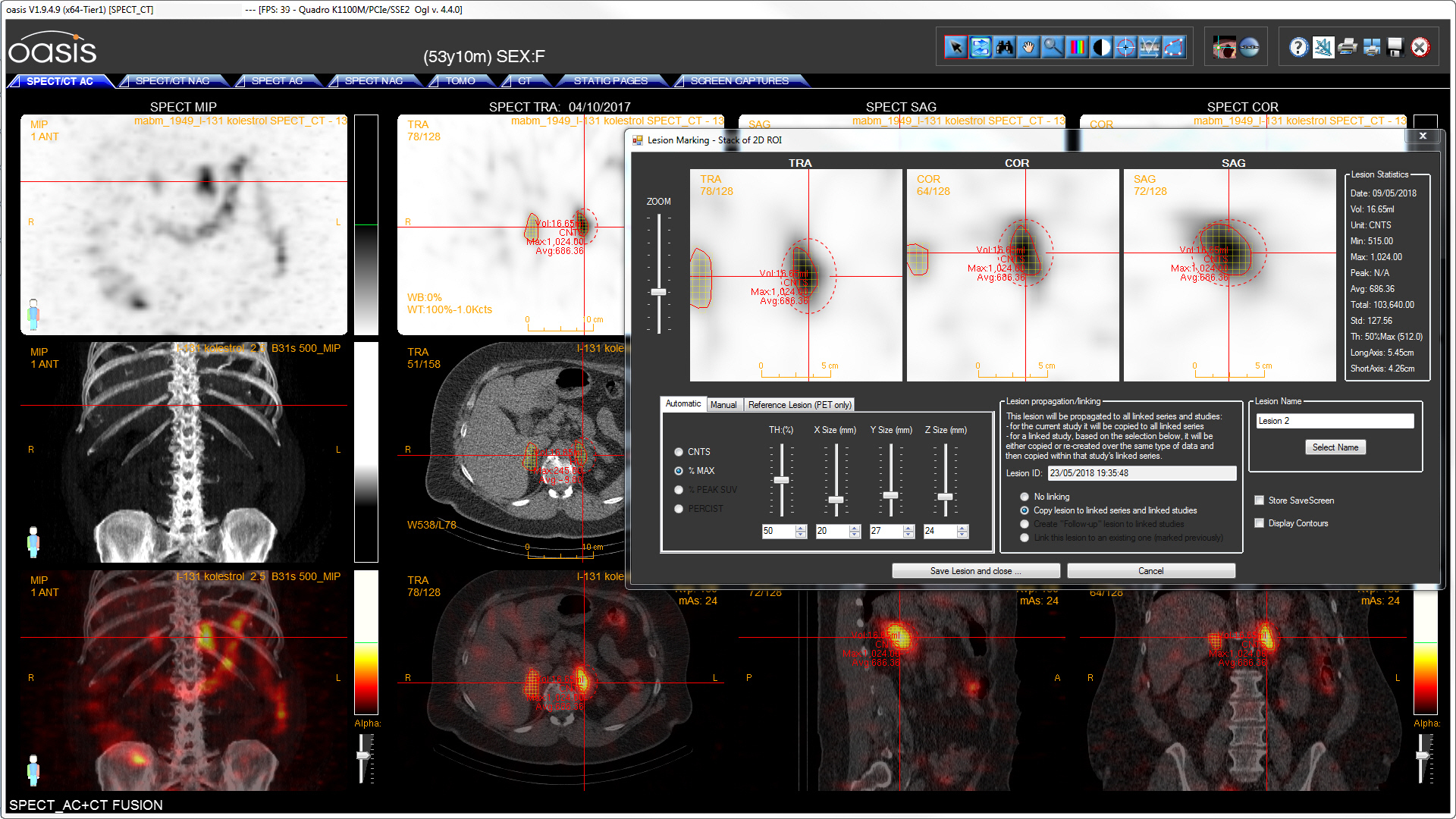
- On a practical level, modern physicians are expected to navigate medical imaging data sets using diagnostic software on their own. In our hospital, traditional radiological demonstration meetings have been scaled back to the minimum. Instead, all physicians have direct access to the PACS. The clinicians’ PACS client includes a diagnostic PET/CT viewer. Due to the new functionality in the viewer, we have stopped creating and saving fused series PET/CT series in our hospital systems. This may not yet be standard practice in other institutions, but we need to educate physicians for the future.
- Hybrid imaging, i.e. morphological imaging such as CT combined with a 3-dimensional acquisition of the distribution of a radioactive tracer, is the central threshold concept behind modern nuclear medicine. The fusion of anatomical and functional information has to be experienced in a practical clinical context in order to be fully understood.
- In our experience, teaching PET/CT is an excellent way of teaching CT, a basic skill that is required by all future physicians. For a newcomer, it can be very frustrating just to find a nodule in a lung CT. If the nodule has tracer uptake in the PET domain, the volume of interest that needs to be scanned for potential CT findings is much smaller.
This analysis has prompted us to shift the focus from mere of knowledge to practical exercises embedded in a clinical context under the new curriculum.
5. Innovating under the new curriculum
With the phasing in of the new curriculum, I started redesigning my courses, one at a time. Since most of these teaching initiatives are published, I aim to be brief.
“Nuclear medicine in endocrinology”. The first module to be taught under new curriculum was the 90-minute seminar on “Nuclear medicine in endocrinology”. I had taught this topic earlier based on my Socratic questioning technique (Biermann 2018), both in the 3rd and the 6th years, but it appeared that my teaching in the 3rd year did not have any lasting effect since I could ask the same questions in the 6th year and still get the same response from the student group.
When redesigning the course, I let myself inspire by team-based learning (TBL). Since the seminar is limited to 90 minutes rather than the three hours recommended for classical TBL sessions, I decided to move the obligatory “Readiness Assessment Test” (RAT) into the LMS. To prepare for the course, students had to watch a 10-minute lecture about thyroid scintigraphy on the UiB website (https://www.uib.no/radionett/nuklear) and answer matching MCQ questions in the university’s new LMS. Students could submit an unlimited number of attempts, receiving detailed formative feedback after each attempt. Canvas LMS has a handy feature that allows a teacher to send personal messages to students who have taken a given quiz and who have not. I used this tool to provide positive feedback to the first responders while sending nag messages to those who lagged behind. For the first time in my teaching career, students were prepared. The 8th term concludes with a full-length examination of about 150 MCQ including questions on nuclear medicine. To prepare students for the MCQ, I prepared a matching set of similar MCQ in the LMS, all including formative feedback (Biermann 2018).
These changes alone had such a profound effect on my teaching that nuclear medicine was awarded the faculty’s 2017 “Teaching Quality Prize”. Still, I saw further potential for improvement. I had developed my variant of “Socratic questioning” by passing a laser pointer around in the audience and asking the student who was in the possession of the pointer increasingly specific questions. Realizing that I only activated one or two students at a time (Biermann 2018), I introduced a classroom response system (Bruff 2009) early in 2018. I chose Socrative (https://socrative.com), which was recommended by the faculty and which proved to be stable inside the wireless network in the lecture hall. Finally, I produced a second online lecture on parathyroid scintigraphy based on student feedback.
“Objective structured clinical examination”. Seeing that traditional university teaching has too much of a focus on the transfer of knowledge but too little on practical skills, I joined the third OSCE pilot in November 2017 by providing a PET/CT station with two of my co-workers. Students had to review a PET/CT study of a patient with lung cancer, demonstrate the lung lesion, judge if the lesion had uptake of the radioactive tracer and was malignant, and prescribe the correct treatment based on the presence or absence of metastases. To prepare students for the OSCE, I created as series of cases in our nuclear medicine teaching database with matching sets of MCQ in the LMS. When I first launched the new OSCE station in autumn 2017, I provided seminars to teach students the use of the PET/CT viewing software. However, the tutorials in the LMS were soon so refined that this was no longer necessary in subsequent years. Under the first OSCE in June 2018, 95 % of all students passed the PET/CT station against the pre-defined objective standard (Gulati et al. 2019).
“Introduction to nuclear medicine”. Based on my experiences with “Nuclear medicine in endocrinology”, I redesigned the 90-minute introductory seminar in the 5th term based on similar principles. This included a pre-seminar RAT in the LMS and Socrative as a classroom response system. Initially, the seminar included 80 students. To provide teaching opportunities for my junior colleagues, I reduced group size to 4 x 40, which is more comfortable to teach, and I optimized my Socrative scripts so that they contain enough clues to the teacher so that the teacher is free to focus on the audience rather than my choreography.
“Nuclear medicine in oncology”. The final new module to be taught under the new curriculum was oncology in the 10th term. The 10th term is special in that the end-of-term MCQ is replaced by a “portfolio examination” (“mappeeksamen”), in which students submit project work. Rather than prepare students for an end-of-term MCQ, my teaching is centered around a mandatory learning activity. While the course module again follows the same general architecture of preparatory online lecture, RAT in the LMS and Socrative as a classroom response system, the learning activity was initially the same teaching material that was used for the OSCE preparation in the 6th term. When the first set of students that had taken part in the OSCE reached the 10th term in autumn 2019, I designed new cases with matching MCQ in the LMS that built on a deeper understanding of oncology (Biermann et al. 2020a). To give students ready access to diagnostic viewing workstations, workstations in the so-called Electronic Patient Journal (EPJ) room in the faculty building were upgraded with wired local area network (LAN) connections to the hospital network since wireless LAN had been too slow.
Elective course “Endocrine surgery: from image to treatment” (ELMED318). Together with Associate Professor Katrin Brauckhoff, endocrine surgeon, and Hans Kristian Haugland, PhD, pathologist, we arranged a two-week elective course at Haukeland University Hospital in January 2018 and in January 2020. Since all three of us are busy enough with our clinical commitments, we chose a flexible course format with just one plenary face-to-face session in the demonstration room of the PET-center from 15:00 to 16:00 h each day. Each day is under a different topic, foundational knowledge being taught in the first week and application in the second week. Students can assist in the operating theater, examine patients in the nuclear medicine or surgery departments using ultrasound, look at cytology preparations of thyroid nodules under a microscope in the pathology department, and study matching cases in the Canvas LMS. We intend to arrange the next course in January 2022.
Teaching under COVID-19. Due to the pandemic, students in the spring term 2020 were locked out from Haukeland University Hospital and the University of Bergen since the beginning of March. This included access to the diagnostic workstations for viewing PET/CT. Rather than roll back our teaching to the old curriculum, we were able to launch a new open source solution for viewing PET/CT within the university network within just 10 days with liberal support from the university’s IT department (Biermann et al. 2020b). In a major effort by the university administration, this time span included regulatory approval. All students managed to conclude their course work despite the lockout. While the first student adopters were enthusiastic about being able to view PET/CT in native format on their own computers at home, students in the survey at the end of the course were more reserved in their approval (Biermann et al. 2020a). As access to teaching facilities continues to be limited, we continue to run the freeware PET/CT viewing solution in parallel with the commercial diagnostic workstations in the faculty building in the current term.
6. Pedagogical theory
To me, the most useful theory for structuring my teaching has been Dee Fink’s theory on significant learning. I was fortunate to meet Dee Fink in person under his seminar at the University of Bergen in 2017. Dee Fink asks us to look for significant, long-lasting learning outcomes: “Have a dream!” What should you students be able understand and do two years after passing your course? Then the course is planned according to the principle of “forward thinking, backward planning”. When we have identified our learning outcomes, we should start planning the examination at the end of our course. The examination should test whether we achieved our intended learning outcomes. When we have planned our examination, we can then plan the rest of our course so that students are able to pass the examination and achieve the intended learning outcomes (Fink 2013).
One of the limitations of Fink’s theory is that the institutional context and in particular the mode of examination is often beyond the control of the teacher (Biggs and Tang 2011). The standard examination at the end of each term under the new medical curriculum is a single five-hour MCQ examination comprising 150 MCQ. As dictated by the national server for medical MCQ at the University of Trondheim (NTNU), the MCQ are to have 3 to 5 alternatives with only a single alternative being correct. In some terms, UiB insists on four alternatives. This is not in line with current literature on MCQ. A large metanalysis has shown that the number of alternatives is not important (Rodriguez 2005). The main challenge when writing MCQ is finding plausible detractors, not the number of alternatives (Parkes and Zimmaro 2016). I prefer the multiple true false pattern (Haladyna 2004 p. 83). Not only does this question type reduce the cognitive load on the student, I argue that this MCQ design is much closer to clinical reality. In clinical practices, there is often fixed number of alternatives (e.g. drug treatment, surgery, radiotherapy, or watchful wait), but several alternatives may be appropriate at the same time. Inspired by Canvas and Moodle LMS, I use a range of question formats in e-learning modules such as numerical and matching questions. Still, even the father of medical MCQ in the United States, Haladyna, has to admit that that OSCE is the gold standard for testing abilities (Downing and Haladyna 2004). I thus use MCQ mainly as a teaching tool to provide timely formative feedback, not as a mode of examination.
The second theory that has guided my teaching since discovering it in 2016, is the Community of Inquiry. The key thesis is that a successful teaching situation has three dimensions: Intellectual presence, teaching presence, and social presence, and that teaching falls flat when one of the three dimensions is lacking (Garrison and Vaughan 2008 sec. 483). Intellectual presence means that the teacher’s and the students’ attention is on the subject matter, not on distractors such as perusing social media while the teacher is droning on. Teaching presence denotes that the teacher is attentive to the students’ progress, providing timely formative feedback. The inclusion of the third element, social presence, may appear to contradict earlier concepts of teaching as a transfer of knowledge. The teacher and students need to be accessible as a social beings, promoting an atmosphere of trust in which students and teacher feel supported. I elaborated on the importance of this third dimension in a course essay on creating an inclusive classroom (Biermann 2018). One of the main challenges of teaching nuclear medicine is that I only meet the students at brief points in their career. Under these circumstances, it is difficult to build up trust. Only if trust is established will a student articulate her deeper thoughts towards a university teacher. I was fortunate to be able to establish some more long-term relationships with selected students that I taught under the transition to the new curriculum. Under the new curriculum, I see students only for 90 minutes at a time. To compensate for this lack of direct student contact, I now make it a point to interact with individual students (often the first adopters, sometimes a struggling student) through the LMS or other channels (Biermann et al. 2020a).
The third theory that has formed me as a teacher is Brookfield’s “Becoming a critically reflective teacher” (Brookfield 2017). The key element is that we should look at our teaching through four “lenses”: the students’ eyes, our colleagues’ eyes, pedagogical literature, and our own experience. As to the latter, the author recommends us to take part as learners in a course on something that we are not good at. In my case, these were sea kayaking and swimming. Being a learner confronts us with our own uncertainties and sometimes anxieties. Hanging under a kayak upside down was most frightening aspect of sea kayaking that I could imagine, and it took me more than half a year to learn the basics of the Eskimo roll (Hutchinson 1999). Likewise, learning front crawl swimming including a flip turn at the end of the swimming lane posed a major challenge to me. Fortunately, I had a very reflective instructor who was able to get me past my anxieties. These experiences help me to be more humble and understanding as a teacher than I normally would be in other professional contexts. They also underline the importance of developing teaching activities that are at once challenging but still doable (Barkley 2010). In swimming instruction, we should not expose people to near drowning but coach them to glide through the water without anxiety (Laughlin and Delves 2012).
My general approach to teaching is based on constructivism. The idea is that you start with something that students already know, that you then take them by surprise by showing them the limits of their knowledge and then help them to construct a new and improved model of the surrounding world. In my course on nuclear medicine in endocrinology, I am aiming for students to understand how to select an appropriate treatment for patients with thyroid disease. In my first course, one student complained that she did not understand. I looked at my teaching materials and found no fault with them, but I had the idea to give her my one-page summary that I had written for nuclear medicine residents. To my surprise, this solved her problem. This episode has taught me that one should give students a choice of learning materials. For teaching PET/CT, I wrote a step-by-step hands-on tutorial in the canvas LMS, but I also recorded a screen cast that shows how to operate the software (https://www.uib.no/radionett/nuklear/undervisning).
Observing myself as a learner, I have hit upon the importance of playing. This is not a new discovery. Interesting enough, the Latin word “ludus” both denotes play and school – there was no distinction. The Dutch philosopher Johan Huizinga built a whole theory about the role of playing in the advance of human culture (Huizinga 1938). To experience flow, play must be fun. When I am trying to pick up new diagnostic approaches such as hybrid PET/MR or a new computer language, my most efficient mode of learning is “playing” with the new data. I think that good learning material should be fun to use – if not all the time, then at least some of the time. I was therefore very happy when 51 % of the students whom I taught nuclear medicine oncology under the COVID-19 pandemic reported that the mandatory PET/CT assignment had been engaging (levels 4 and 5 on a 5-point Likert scale ranging from “fun” to “tedious”) (Biermann et al. 2020a).
In his monumental metaanalysis on teaching methods, Hattie concluded that no single method is “best”, but that lasting learning occurs when the learner reflects on her own learning (Hattie 2010). This mechanism is operative under group learning: The more advanced group member tries to find out what is the stumbling block in the struggling learner and thus starts reflecting on a higher level while the learner gets an explanation that best addresses her immediate needs. I realize that my teaching material may not be challenging enough for the most advanced students. I therefore ask them to find the mistakes in my teaching material and argue for their observations. I regard letting students outsmart the professor as a very powerful engagement technique (Barkley 2010).
One of the “Bibles” of internal medicine during my medical studies made the point in the opening chapters that medicine was all at once science, art, and a craft (Cecil et al. 1988). The same applies to pedagogy. I often use sports analogies to visualize scientific or pedagogical challenges. Since I try to perform as instructor on a competitive level, my self-adopted teaching motto has become:
Teaching is like decathlon: To take a medal, you must excel in two disciplines. But one major dropout in the others will take you down.[1]
Even if I may excel by using advanced e-learning tools and live data embedded in a meaningful clinical context, I still have to make sure that everybody is prepared, everybody comes on time, and that the presentation technology and the auditorium meet all requirements. If the video projector is not working or the network is down, it will kill the whole session. The purpose of my motto is to keep me firmly grounded and make sure that I continue to pay attention to nitty gritty details such as testing the auditorium two days ahead of a teaching session.
7. E-learning
The biggest innovation in university teaching in the recent two decades has been e-learning – to the extent that it seems to upend the normal laws of pedagogy. This is however not true.
Robert Gray at the University of Bergen taught me the basics of e-learning. One of his core statements is that e-learning was developed alongside social media primarily to save money so that students could be taught in larger groups. A second aspect was making education more accessible to students in remote areas (Haslerud et al. 2017). It appears that pedagogy came last – with the exception of a few visionaries like Martin Dougiamas, the founder of moodle.org.
Just because we teach in an electronic space does not mean that the normal principles of teaching do not apply. Indeed, successful e-learning requires the same general approach as teaching in other contexts. Pedagogy should come first, technology second.
Teaching materials do not need to perfect. Perfection can be paralyzing to the audience. I found that not striving for perfection in my learning materials gives me more creative freedom. Also, I, the teacher, is permitted to make mistakes. It also helps me to use my limited time more effectively. It even gives me a new technique to engage my highest performing students. Since I design my materials for the average student, my teaching material may be too simple for some or just simply boring. When I asked them to find the errors in my teaching material, they need to sharpen their perception so that they can beat me, the professor, at my own game. The resulting discussions are always very rewarding both for the student and for myself. This because reflecting on one’s own learning is the most efficient teaching technique (Hattie 2010).
My general teaching motto still applies: The technological details need to be in place for e-learning to succeed. An LMS needs to be responsive, and courses need to be easy and ergonomic to navigate.
My initial choice of Moodle LMS, the system that we introduced for training of nuclear medicine residents in 2015 (Biermann 2016), was opportunistic. Having ample experience with Linux – Apache – PHP – MySQL (LAMP) frameworks (Biermann 2014), I saw that Moodle had a small footprint and was easy to roll out in the context of the hospital’s IT infrastructure. Only later I came to realize the hidden power of Moodle, which is supported by a world-wide community of e-learning enthusiasts. Moodle comes with many indispensable plug-ins. One the most useful is “Collapsed topics”, which prevents the “scroll of death” in extended courses with many items (Barnard 2016).
An underappreciated aspect of LMS is the quality of the authoring tools. Under Moodle LMS, an interactive case takes about 1 – 2 hours to design, not the least because Moodle LMS permits the cloning of questions within the questions database. Under UiB’s current implementation of Canvas LMS, attempting to clone questions leads to unpredictable results.[2]
Drawing on my background as a developer (Biermann 2014), I emphasize the virtues of modular e-course design (Biermann 2016; Biermann et al. 2020a; Gulati et al. 2019): In a modular e-learning architecture, individual modules can be replaced (such as the PET/CT viewing software under the pandemic) without having to redesign the whole course (Biermann et al. 2020a).
The latest trend in e-learning is called gamification (Denmeade 2015). At first, I misunderstood and thought that gamification meant the trivialization of serious academic content. However, the main point is motivating the audience by introducing elements of achievement. Seen from yet another angle, gamification is also about usability and modern user interface design. An electronic course should be user-friendly and easy to navigate. Like in good computer game, the user interface should be intuitive, clear, and simple to enhance user experience. There should be no complicated menus to distract from the game. As an experiment, I gamified our e-course in nuclear medicine NM5, introducing self-designed badges for student and teacher achievement in December 2019, but I have not yet accumulated enough feedback in order to judge whether the effort was worthwhile.
8. Ongoing projects
The Norwegian system for training medical specialists has been undergoing a major reform (Haslerud et al. 2017). Under the old system monitored by the Norwegian Physicians’ Association (Dnlf), training in nuclear medicine took five years, of which at least three were spent in a department of nuclear medicine. There was no final examination, but fellows had to perform a stipulated number of procedures and attend a specified number of obligatory and elective courses totaling 210 hours of course education. The new system is based on detailed learning outcomes specified for each medical specialty (Spesialistforskriften 2016). Being the leader of the Nuclear Medicine committee (Spesialitetskomiteen) since 2014, I was in the midst of these changes.
Following the reform, two extra nuclear medicine courses were introduced: NM4 “Practical nuclear medicine: organ diagnostics” and NM5 “Practical nuclear medicine: oncology”. Since there are only about 25 nuclear medicine fellows and 35 nuclear medicine specialists active in the specialty, plenary courses are very demanding to arrange. When expanding the catalog of obligatory nuclear medicine courses from 90 to 150 hours, we therefore put an emphasis on e-learning in order to contain costs. The two new courses NM4 and NM5 are therefore arranged as e-learning courses in our own LMS (https://nukit.ihelse.net/moodle) (Biermann 2016). The LMS is exposed to the Internet so that residents and teachers can log on from their personal computers at home or from their mobile devices.
To make the new e-courses a success in the nuclear medicine community, course design had to be standardized so that both students and teachers would know what was expected from them. A typical nuclear medicine course day therefore always has the same structure. It is opened by a 30-minute life lecture shared through a videoconferencing system (https://whereby.com). A recording of the lecture will be put out on the Moodle LMS. Each lecture is supplemented by a set of mandatory learning activities. The students need to answer simple questions about the lecture. The second module consists of two selected open access articles that are relevant to the topic with matching MCQ questions. Finally, students course participants are required to process and read one or two cases from our national teaching database https://nukoa.ihelse.net in the Norwegain Health Network in diagnostic hybrid format and answer matching MCQ questions in the Moodle LMS. When all MCQ modules are passed with at least 80%, the Moodle feedback module will open in which students can rate their satisfaction with the present course module including free text comments. This will be important when we arrange the courses for the next time. As per September 2020, NM5 is nearly completed while NM4 will be arranged in 2021.
We also reevaluated our previous course in clinical nuclear medicine. In 2016, this was a plenary course which included thirty 45-minute lectures. Interactive activities and group work based on our new Moodle LMS in the afternoons happened after the obligatory course activities with variable attendance (Haslerud et al. 2017).
Based on our experiences in 2016, we redesigned the course NM3, which was to be held in November 2020. Instead of 30 lectures, we plan ten three-hour thematic blocks. In our original plans students and teachers were to meet in a specially equipped computer lab at E-helse Bergen, which has fifteen 3-screen diagnostic PACS workstations. Each session would be introduced by a short (10 minute) lecture. Then groups of 2 to 3 students, one experienced and one less experience from two different centers would process matching nuclear medicine examinations in native format guided by information and questions in the Moodle LMS. While the new course format had already been approved both by the Norwegian Physicians’ Association and the regional training centers, the ongoing pandemic forces us to replace the face-to-face course in Bergen by a fully electronic meeting early in 2021.
9. Conclusions
The above outlined my development as a university teacher: My initial teaching fell flat since I focused too much on transferring knowledge and optimizing content delivery. Only when I started aiming for rich learning outcomes with an emphasis on clinical reasoning and practical competencies in conjunction with the new medical curriculum at the University of Bergen and a liberal injection of formal pedagogical education, did I achieve student and teacher satisfaction. I hope that this journey will serve to inspire other university teachers who are facing similar challenges in their respective domains.
Footnotes
[1] You find it on this website under “Teaching philosophy”
[2] Also Canvas LMS is open source. I posted the issue on the relevant forum in 2019, but got no reply.
References
Barkley, E.F., 2010. Student engagement techniques: a handbook for college faculty, The Jossey-Bass higher and adult education series. Jossey-Bass, San Francisco. ISBN 978-0-470-28191-8.
Barnard, G.J., 2016. The complete guide to collapsed topics. Blurb, London. ISBN 978-1-364-32544-2.
Biermann, M., 2018. Building an inclusive classroom – a blended course in Nuclear Medicine. UPED-Skrift 2018, 1–8. https://doi.org/10.13140/RG.2.2.26883.76321
Biermann, M., 2016. A national e-learning platform for training specialists in Nuclear Medicine in Norway. UPED-Skrift 20156, 7. https://doi.org/10.13140/RG.2.1.3467.8162
Biermann, M., 2014. A simple versatile solution for collecting multidimensional clinical data based on the CakePHP web application framework. Comput Methods Programs Biomed 114, 70–79. https://doi.org/10.1016/j.cmpb.2014.01.007
Biermann, M., Kanoun, S., Davidsen, T., Gray, R.Jr., 2020a. An Open Source Solution for “Hands-on” teaching of PET/CT to Medical Students under the COVID-19 Pandemic. Nuklearmedizin (accepted).
Biermann, M., Kanoun, S., Davidsen, T., Gray, R.Jr., 2020b. Teaching PET/CT to medical students under the COVID-19 lockout: Implementing a new freeware client server PET/CT viewer in the university network (Abstract; oral presentation 884). Eur J Nucl Med Mol Imaging 47, S437-8.
Biggs, J.B., Tang, C.S., 2011. Teaching for quality learning at university: what the student does, 4. ed., SRHE and Open University Press imprint. McGraw-Hill, Society for Research into Higher Education & Open University Press, Maidenhead. ISBN 978-0-335-24275-7.
Brookfield, S., 2017. Becoming a critically reflective teacher, Second edition. Jossey-Bass, San Francisco, CA. ISBN 978-1-119-04970-8.
Bruff, D., 2009. Teaching with classroom response systems: creating active learning environments, 1st ed., The Jossey-Bass higher and adult education series. Jossey-Bass, San Francisco. ISBN 978-0-470-28893-1.
Cecil, R.L., Wyngaarden, J.B., Smith, L.H. (Eds.), 1988. Textbook of medicine, 18th ed. Saunders, Philadelphia. ISBN 978-0-7216-1848-7.
Denmeade, N., 2015. Gamification with Moodle: use game elements in Moodle courses to build learner resilience and motivation. Packt Publishing Limited, Birmingham. ISBN 978-1-78217-307-6.
Downing, S.M., Haladyna, T.M., 2004. Validity threats: overcoming interference with proposed interpretations of assessment data. Medical Education 38, 327–333. https://doi.org/10.1046/j.1365-2923.2004.01777.x
Fink, L.D., 2013. Creating significant learning experiences: an integrated approach to designing college courses, Jossey-Bass Higher and Adult Education Series. Jossey-Bass, San Francisco. ISBN 978-1-118-12425-3.
Garrison, D.R., Vaughan, N.D., 2008. Blended learning in higher education: framework, principles, and guidelines, 1st ed., The Jossey-Bass higher and adult education series. Jossey-Bass, San Francisco. ISBN 978-0-7879-8770-1.
Gulati, A., Schwarzlmüller, T., du Plessis, E., Søfteland, E., Gray, R., Biermann, M., 2019. Evaluation of a new e-learning framework for teaching nuclear medicine and radiology to undergraduate medical students. Acta Radiologica Open 8, 205846011986023. https://doi.org/10.1177/2058460119860231
Haagensen, R., Olsen, K.A., 2003. RABILDA. Evaluation of an eLearning System for Radiology. Presented at the Norwegian Informatics Conference, Norwegian Informatics Conference, Oslo/Norway.
Haladyna, T.M., 2004. Developing and validating multiple-choice test items, 3rd ed. Lawrence Erlbaum Associates, Mahwah, N.J. ISBN 978-0-8058-4661-4.
Haslerud, T., Tulipan, A.J., Gray, R.M., Biermann, M., 2017. E-learning for medical imaging specialists: introducing blended learning in a nuclear medicine specialist course. Acta Radiologica Open 6, 205846011772085. https://doi.org/10.1177/2058460117720858
Hattie, J.A.C., 2010. Visible learning: a synthesis of over 800 meta-analyses relating to achievement, Reprinted. Routledge, London. ISBN 978-0-203-88733-2.
Huizinga, J., 1938. Homo ludens: Proeve ener bepaling van het spelelement der cultuur. Wolters-Noordhoff, Groningen.
Hutchinson, D.C., 1999. Derek Hutchinson’s guide to eskimo rolling. A. & C. Black, London. ISBN 0-7136-5108-3.
Laughlin, T., Delves, J., 2012. Total Immersion: the Revolutionary Way to Swim Better, Faster, and Easier. Touchstone, New York. ISBN 978-1-4516-8833-7.
Parkes, J., Zimmaro, D., 2016. Learning and assessing with multiple-choice questions in college classrooms. Routledge, Taylor & Francis Group, New York. ISBN 978-1-138-84597-8.
Rodriguez, M.C., 2005. Three Options Are Optimal for Multiple-Choice Items: A Meta-Analysis of 80 Years of Research. Educational Measurement: Issues and Practice 24, 3–13. https://doi.org/10.1111/j.1745-3992.2005.00006.x
Rootwelt, K., 2005. Nukleærmedisin. Gyldendal Akademisk, Oslo. ISBN 82-05-31118-8.
Spesialistforskriften, 2016.
Wictionary, 2020. Unclear Medicine. Wictionary.org.